We have a saying at home and around the office that we invoke whenever we learn something new: “You don’t know what you don’t know until you don’t know it.” And surely it is true that you can’t possibly know something that you have never been exposed to — isn’t it?
All the same, this idea can be a two-edged sword, because clearly there are some things that we should know thanks to education or experience — or because a partner, spouse, parent, or friend has told it to us so many times that claiming not to know is akin to a death wish. Tuesday is trash pick-up. Your mother’s birthday falls on the same date each year. Forget that sort of thing at your peril.
The other day I encountered a situation that made me stop and re-examine some assumptions I’d made about what my clients knew, vs. what they really had been exposed to or learned from work|life experience.
I was coaching a nurse who had recently left bedside nursing to work in informatics, specifically with clinical outcome data and quality reporting. As we were going through the information, she stopped me and said, “you know, I have seen these reports posted on the hospital floor over the years, but I never understood what ‘infection rate per thousand’ means and no one ever explained it to me — can you please explain it?” (I want to acknowledge and applaud the courage it took for this nurse to say this.)
I was more than happy to oblige, so we talked about those rates at length. Understanding them is really important in successful interpretation of clinical outcome data and its contribution to performance improvement.
Here is a summary of my tutorial.
What is a rate? A rate is like a ratio, except that it compares two quantities with different units: the number of infections observed in a hospital, for example, out of the total population at risk.
Why and how do we calculate rates? We calculate rates so that we can make fair and correct comparisons, and to identify solid opportunities for improvement. Consider, for example, the consequences of reporting only the number of urinary-tract infections (UTI’s) in the month of April at Hospital A as 55 versus 25 at Hospital B. (As opposed to comparing them in the context of the entire at-risk population.) Upon reading the number of UTI’s in isolation, we could conclude that Hospital A was performing worse than B. But that might not be true. We have to consider the denominator — the other unit besides “number of infections”– at both hospitals. In this case, the denominator (the other unit in the rate), would be the population at risk for infection.
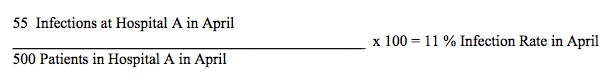
For example, if the number of patients at risk for at Hospital A is 500, and at Hospital B 100, then the infection rate for April would be 11% [(55/500) x 100] at A and 25% [(25/100) x 100] at B — and that is a very different story from the one we first narrated by simply reporting the infection count.
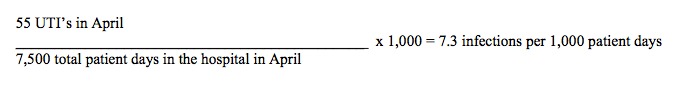
Another way that infection rates are often calculated and displayed is by using the number of patient days; that is, each patient’s number of days in the hospital summed for the total population at risk. This method gives us even better information than the previous rate, because it accounts for all of the time (number of days) that patients were in a hospital and therefore at risk for infection. Let’s assume that the 500 patients in the first example were in the hospital for a total of 7,500 days in April:
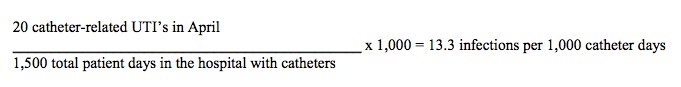
In an example like the one I have been using, incidence rates can be further defined to match specific medical devices (I chose UTI’s as my example for a reason). To calculate the incidence of UTI’s related to urinary tract catheterization, we would include only the number of patient days during which patients had a catheter in place, further refining the population at risk. Let’s express this with the following formula:
As you can see, understanding what rates are, how to build them, and why they’re useful and important is crucial to identifying both areas needing and methods to achieve improvement. The first rate cited above gave us an idea that there was a problem with UTI’s, but told us little beyond that. Then, as we refined our patients at risk via the denominator, we were able get a clearer picture of the size and scope of the problem, and to take specific steps toward improvement that precisely targeted — and most helped-those patients at greatest risk.
Perhaps best of all, pulling out paper and pencil to explain all this to a nurse who was brave enough to ask brought me a really important and valuable insight: I hadn’t known what she didn’t know. Finding that out helped both of us challenge our assumptions, reduce confusion and enhance clarity, and do a better job of serving those who needed us.


0 Comments