When is a world record marathon time not a world record marathon time? When there are hills involved.
On April 18th a 29-year old Kenyan named Geoffrey Mutai completed the Boston Marathon nearly one entire minute faster than the recognized marathon record of 2:03:59 that Ethiopia’s Haile Gerselaissie established for the same distance on Berlin’s flat course in 2008.
But here is the rub — although the International Association of Athletics Federation (IAAF) includes Boston performances on its all-time list and acknowledges on its website that Mutai’s time is the “fastest marathon ever,” the federation will not recognize it as a world record because the course, by its standards, has an excessive elevation drop.
Take a look at the following graphic shows the difference in several other marathon courses as compared with Boston:
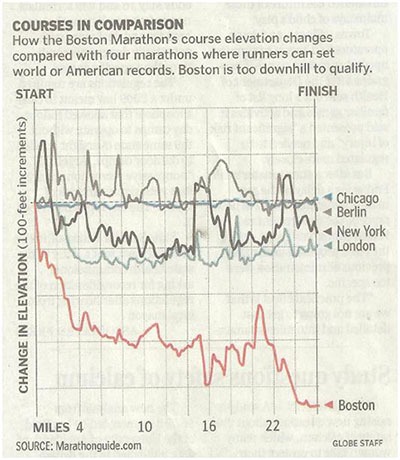
Source: April 29, 2011 Boston Globe
Now I am not interested in all of this because I am a runner or even because I love to watch the marathon (I can walk right down the hill from my house to see the race which is a very good thing because I wouldn’t want to have to exert too much energy going to watch it) rather, I find this turn of events interesting as I think about the importance of properly risk-adjusting healthcare data.
Just like it makes sense to try and keep marathon world records fair by adjusting for the difficulty of a course in comparison to other courses, it also only makes sense to adjust healthcare data based on the unique characteristics that patients bring to their healthcare encounters and the types of treatments or procedures they are undergoing (among other factors).
Risk-adjustment levels the playing field and allows for “apples to apples” comparisons.
Consider the following visualization of adjusted versus unadjusted mortality rates based on the National Surgical Quality Improvement Program (NSQIP) — the seminal work in risk-adjusted surgical outcome and quality improvement of Shukri Khuri, M.D., Jennifer Daley, M.D. and William Henderson, Ph.D. (the finest group of people I have ever had the privilege of working with — and I have worked with some pretty great people).
Drs. Khuri and Daley often used this visualization to demonstrate the importance of risk-adjustment. The left hand column ranks medical centers (small blue dots) based on the number of surgical mortalities observed by each institution — completely unadjusted data. Now look at the lines across the visual which show the change to each medical center’s ranking after adjusting the mortality rates for patients unique risks and the types of procedures performed (expressed as the Observed versus Expected Ratio — the “expected” having been modeled and calculated from NSQIP data). The red and orange dots and lines are highlighted examples to show just how significantly a center’s ranking can change after risk-adjustment.
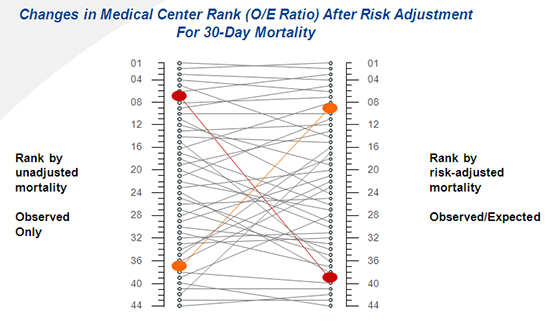
Source: Drs. Khuri, Daley, Henderson VHA NSQIP
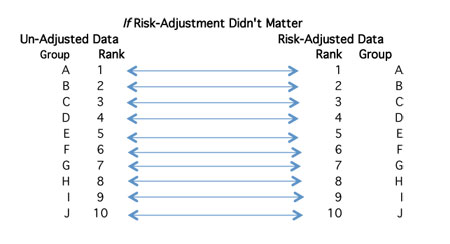
If risk-adjustment didn’t matter this graph would look like a railroad track.
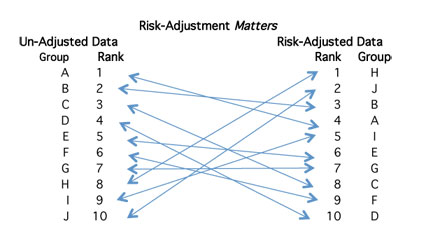
BUT, risk-adjustment matters as demonstrated by the change in the medical centers ranking after risk-adjustment.
Clearly failure to adjust data for patients’ risks carries consequences much greater than the embarrassment of incorrectly reported data. In the current healthcare environment, where quality and outcomes are increasingly linked to reimbursement and public reporting initiatives risk-adjustment is essential to ensure that you:
- Know how the reporting accounts for different factors that could affect the outcomes of patients’ encounters and procedures.
- Appropriately identify the correct opportunities for improvement.
- Gain stakeholder buy-in to the changes.
- Include adequate risk-adjustment methodologies into your pay-for-performance contracts.
But understanding and communicating how data is risk-adjusted is a challenge. Can you and your team confidently explain to all of your stakeholders:
- The importance of risk-adjustment and the consequences of failing to adequately account for patients’ risks?
- The different dimensions of risks and how they vary depending upon the outcomes being measured?
- The available data sources for risk-adjustment and the implications of using them?
- The characteristics, strengths and limitations of risk-adjustment development and methodology?
- The validity and efficacy of a risk-adjustment method?
- The reliability of risk-adjustment methodology and factors to consider in evaluating the reliability of a risk model?
So, what’s your plan to fully understand risk-adjustment of healthcare data and to communicate it to all of your stakeholders?


0 Comments